Advanced liver disease
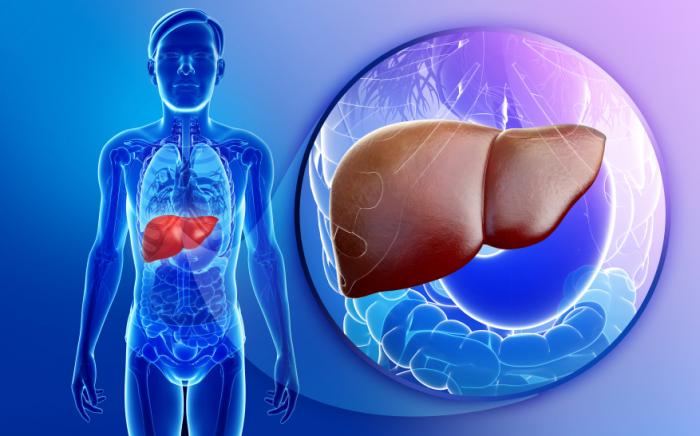
Portal hypertension is a complication that arises when scar tissue in the liver blocks blood flow. This causes increased pressure in the portal vein, which can lead to enlarged veins in the esophagus or stomach (varices), and dangerous internal bleeding. Symptoms may include vomiting blood or black, tarry stools. Treatment often involves medications, procedures to reduce pressure, or surgery.
Ascites is another complication of advanced liver disease. This condition involves the buildup of fluid in the abdomen, causing swelling and discomfort. It’s often accompanied by weight gain, bloating, and shortness of breath. Managing ascites may involve dietary changes, diuretics, or drainage procedures, depending on the severity.
How Mental health Suffers
 Mental health often suffers in people living with chronic liver disease. Depression, anxiety, and cognitive impairment can result from both the physical toll of liver dysfunction and the emotional stress of dealing with a long-term illness. Integrated care that includes mental health support is essential for managing liver disease holistically.
Mental health often suffers in people living with chronic liver disease. Depression, anxiety, and cognitive impairment can result from both the physical toll of liver dysfunction and the emotional stress of dealing with a long-term illness. Integrated care that includes mental health support is essential for managing liver disease holistically.
Liver disease can affect brain function through a condition known as hepatic encephalopathy. When the liver fails to filter toxins effectively, substances like ammonia accumulate and affect the brain. This can lead to confusion, personality changes, drowsiness, and in severe cases, coma. Prompt treatment is essential to reverse symptoms and prevent long-term damage.
Liver transplants can be lifesaving
 Liver transplants can be lifesaving for individuals with end-stage liver disease. The procedure involves replacing a diseased liver with a healthy one from a donor. Candidates must undergo extensive evaluation and be added to a transplant waiting list. Post-transplant care includes lifelong medication to prevent organ rejection and regular follow-ups to monitor liver function.
Liver transplants can be lifesaving for individuals with end-stage liver disease. The procedure involves replacing a diseased liver with a healthy one from a donor. Candidates must undergo extensive evaluation and be added to a transplant waiting list. Post-transplant care includes lifelong medication to prevent organ rejection and regular follow-ups to monitor liver function.
Alcohol-related liver disease (ARLD) remains one of the most preventable forms of liver damage. Long-term heavy drinking causes fat buildup, inflammation, and scarring in the liver. The progression from fatty liver to alcoholic hepatitis and eventually cirrhosis can often be reversed if alcohol use is stopped early, but becomes harder to treat in later stages.
Unique challenges with liver disease
 Women may face unique challenges with liver disease. For instance, hormonal fluctuations during pregnancy can worsen liver conditions, and diseases like autoimmune hepatitis are more common in women. Additionally, women may be more susceptible to alcohol-related liver damage than men, even with lower alcohol intake, due to biological differences in metabolism.
Women may face unique challenges with liver disease. For instance, hormonal fluctuations during pregnancy can worsen liver conditions, and diseases like autoimmune hepatitis are more common in women. Additionally, women may be more susceptible to alcohol-related liver damage than men, even with lower alcohol intake, due to biological differences in metabolism.
The liver has a remarkable capacity for regeneration. Even after significant damage, liver tissue can heal if the cause is addressed. However, this ability has limits—once scarring becomes extensive (as in cirrhosis), the liver can no longer fully regenerate. Early detection and intervention are key to preserving this regenerative power.
Factors can increase liver disease risk.
 Certain occupations can increase liver disease risk. People exposed to industrial solvents, heavy metals, and pesticides may be at higher risk for developing toxic liver injury. Protective gear and regular medical screenings are important for workers in high-risk industries like agriculture, chemical manufacturing, and dry cleaning.
Certain occupations can increase liver disease risk. People exposed to industrial solvents, heavy metals, and pesticides may be at higher risk for developing toxic liver injury. Protective gear and regular medical screenings are important for workers in high-risk industries like agriculture, chemical manufacturing, and dry cleaning.
Dietary choices significantly impact liver health. A diet rich in vegetables, lean proteins, whole grains, and healthy fats can reduce liver fat and inflammation. Foods like leafy greens, berries, nuts, and fish rich in omega-3s are liver-friendly. Avoiding processed foods, sugary beverages, and trans fats is essential for preventing or managing liver disease.
Special care for People with Liver Disease
 People with liver disease must take special care with medications. The liver processes most drugs, so impaired function can affect how medications are metabolized. This can lead to increased side effects or toxicity. Always consult a healthcare provider before starting new medications or supplements, especially with chronic liver conditions.
People with liver disease must take special care with medications. The liver processes most drugs, so impaired function can affect how medications are metabolized. This can lead to increased side effects or toxicity. Always consult a healthcare provider before starting new medications or supplements, especially with chronic liver conditions.
Travelers should be aware of liver disease risks, particularly in areas with poor sanitation. Hepatitis A and E are transmitted through contaminated food and water. Vaccination, hand hygiene, and safe food practices are vital for prevention. Those with existing liver disease are especially vulnerable to complications from hepatitis infections.